Bulging Disc Symptoms, Causes and Treatments Options
Disc prolapse, also commonly known as bulging or herniated disc is a condition where the gel-like center in between any two vertebrae of the spine called the disc, bulges out into the spinal canal causing compression of its nerve roots. It is twice more prevalent amongst men compared to women and is one of the most frequently seen abnormalities leading to back pain in people aged 30-50 years, with an incidence of 5-20 cases per 1000 adults annually.
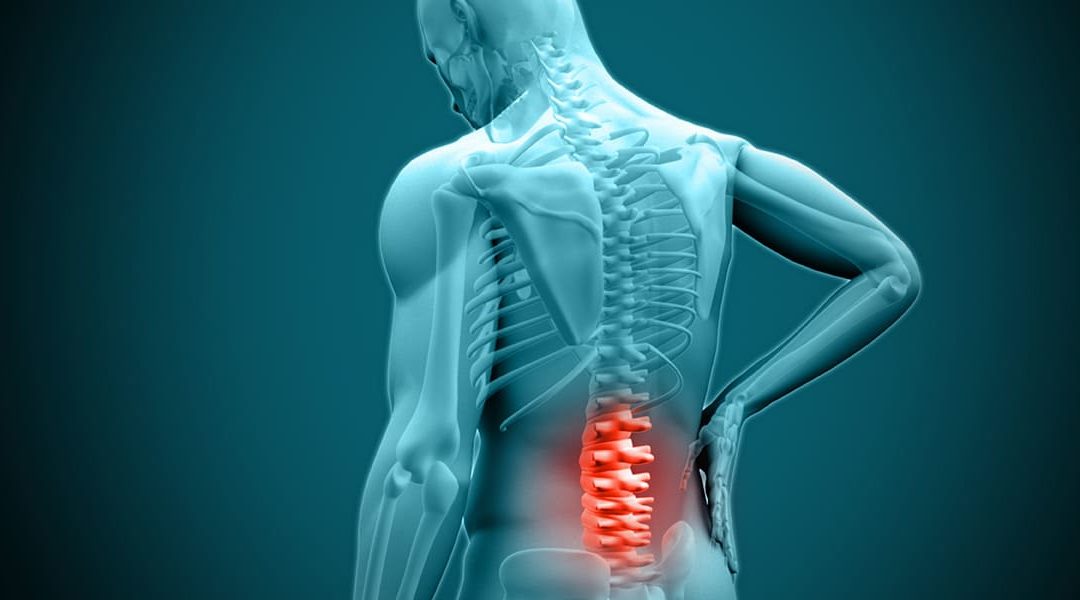
Bulging of the disc can generally involve any level of spinal vertebrae from the neck to the lower back, however involvement of the lumbar region is more predominantly noticed. Depending on the severity and the level of prolapse, the range of symptoms may vary from very mild pain to severe shooting type of pain associated with numbness or neurological weakness.
Causes & Risk factors
Disc herniation usually occurs due to age-related wear and tear of the disc leading to its degeneration. This degeneration leads to weakening of the outer layer of the disc called annulus fibrosis resulting in the inner jelly-like portion called nucleus pulposus to herniate out. The other relatively uncommon cause of herniated disc is due to a traumatic event with sudden jerking movement that leads to undue pressure on the disc resulting in prolapse.
There are multiple factors which may increase the risk of disc prolapse like increasing age which may reduce the flexibility of the disc due to loss of its water content, male sex, obesity, smoking, lifting heavy weights, professional athletes due to blunt impact trauma, poor posture, frequent driving due to its undue pressure on the spine and sedentary lifestyle habits.
Symptoms
One of the most widely seen symptoms of disc bulge is lower back pain. People may also present with complaints of neck pain or stiffness, pain in the buttocks or hips, numbness or tingling sensation of the neck, back, arms, hands, legs or feet, and muscle weakness. These various symptoms associated with prolapse generally depend on the level of the spinal vertebrae involved, the size of the disc bulge, and its severity based on nerve root compression.
However, a majority of patients may also remain asymptomatic or have very mild symptoms as the size of the prolapse remains constant for a long time.
Diagnosis
Medical physical examination by a doctor to assess the region of pain, its intensity, muscle weakness, loss of sensation and the range of physical activity plays a crucial role in the diagnosis of a suspicious disc herniation. However, MRI imaging of the spine remains the gold standard investigation recommended in the accurate diagnosis of a disc bulge, its level of involvement and the severity of nerve root compression.
Occasionally since some people with symptoms of disc prolapse may improve in 4-6 weeks duration without any major treatment, imaging studies like MRI tends to add more value in those with sudden severe pain, traumatic event or during evaluation for surgical intervention.
Other modalities of investigations generally advised include, X-ray to rule out other causes of pain, CT scans when MRI is not feasible, electromyelogram & myelogram to assess the effects and level of nerve compression.
Treatment
People with mild symptoms that don't affect day-to-day activities are generally managed with rest, pain killers, anti-inflammatory medications, steroid injections and physical therapy.
Despite conservative non-surgical management for 4-6 weeks, some people may have worsening of symptoms, like pain, muscle weakness, difficulty walking, sudden loss of sensation including bowel or bladder control and require emergency surgical intervention.
Multiple surgical options to relieve the pressure on the nerve roots are available like decompression, discectomy, laminectomy, spinal fusion or artificial disc surgery. In addition to the traditional surgical options, recent advancements like minimally invasive microdiscectomy procedures have resulted in highly successful outcomes, minimal discomfort post-surgery and relatively faster surgical recovery.
Prevention
Though there are no certain ways of preventing a disc prolapse, it is generally recommended that maintaining a healthy weight and active lifestyle, good posture, avoiding use of tobacco products and regular exercise not only help reduce the chances of having a disc prolapse but also reduces the risk of recurrence or worsening of symptoms in people with mild or asymptomatic disease.
